
KEN ISHII, MD, PhD
Spine & Spinal cord Surgeon
Specialist in Anti-Aging Medicine
- About Dr. KEN ISHII
- PROFESSIONAL APPOINTMENTS
- APPOINTMENTS
- EDUCATION
- HONORS/ AWARDS
- EDITORIAL BOARD
- CLINICAL ACHIEVEMENTS
- SURGICAL COMPLICATION RATES of Dr. Ishii`s PROCEDURES (Past 5 years)
- FACULTY EXPERIENCE at INTERNATINAL MEDICAL INSTITUIONS
- PUBLICATIONS & PRESENTATIONS
- Pathophysiology, Diagnosis, Treatment, and Rehabilitation (SHAiR Program) of Dropped Head Syndrome
About Dr. KEN ISHII
Dr. Ken Ishii is a world-renowned spine and spinal cord surgeon representing the Asia-Pacific region. After graduating from Keio University School of Medicine, Japan, in 1993, he pursued a career as an orthopedic surgeon. Dr. Ishii completed his training in orthopaedics at Keio University and worked in clinical and regenerative medicine at Georgetown University and Massachusetts General Hospital (MGH)/ Harvard University in the United States from 2000 for about four years.
In 2015, Dr. Ishii was appointed as the chief of the Spine Team at the Department of Orthopedic Surgery at Keio University School of Medicine. In 2017, he assumed the first chairman & professor of Orthopedic Surgery at the International University of Health and Welfare, and in 2023, he was appointed as a Designated Professor at Keio University School of Medicine. During his tenure as a university professor, he made significant contributions not only in clinical practice but also in basic research, education, and academic activities, both in Japan and internationally. In late 2023, Dr. Ishii took on the position of Chief Director at New Spine Clinic Tokyo. Throughout his career, Dr. Ishii has received numerous prestigious awards in recognition of his achievements.
In 2010, he was honored with the Best Poster Award at the 1st Meeting of the Cervical Spine Research Society Asia-Pacific Section (CSRS-AP), the first-ever CSRS-AP meeting held in the Asia-Pacific region. In 2012, he received The Encouragement Award (Clinical Research) from The Japanese Orthopaedic Association (JOA), one of Japan’s most prestigious orthopedic awards. He was also awarded The Guest Nation Poster Award from The American Academy of Orthopaedic Surgeons (AAOS) 2012, the most historically significant and authoritative orthopedic society in the world. In 2015, Dr. Ishii was selected for The Cervical Spine Research Society (CSRS) Traveling Fellowship, where he represented Asia in fostering exchanges with top spine surgeons from North America and Europe.
Dr. Ishii continues to lead advancements in spinal surgery worldwide, collaborating with international experts and contributing to the evolution of minimally invasive spinal treatments.
PROFESSIONAL APPOINTMENTS
- 1993
- Resident, Department of Orthopaedic Surgery, Keio University School of Medicine
- 2009
- Assistant Professor, Department of Orthopaedic Surgery, Keio University School of Medicine
- 2017
- Designated Professor, Keio University School of Medicine
- 2017
- Professor and Chairman, Department of Orthopaedic Surgery, School of Medicine, International University of Health and Welfare (IUHW)
- 2023
- Designated Professor, Department of Orthopaedic Surgery, Keio University School of Medicine
Director, New Spine Clinic Tokyo (NSC Tokyo)
APPOINTMENTS
- Board certified orthopaedic surgeon
- Certified specialist in spine and spinal cord diseases
- Specialist in cervical & lumbar diseases
- Certified specialist in dropped head syndrome (DHS) by the DHS Association
- Certified spinal endoscopic surgeon
- Specialist for minimally invasive spinal treatment
- Specialist for spine & spinal cord tumors
- Board director of the Cervical Spine Research Society Asia-Pacific Section (CSRS-AP)
- Member of Cervical Spine Research Society (CSRS)
- Board director of the Minimally Invasive Spinal Treatment (MIST)
- Councilor of the Japanese Society of Anti-Aging Medicine (JAAM)
- Member of International Society for the Study of the Lumbar Spine (ISSLS), etc.
EDUCATION
- 1993
- M.D. Keio University School of Medicine
- 2002
- Ph.D. Keio University School of Medicine
- 2000-2002
- Postdoctoral Fellow, Department of Neuroscience, Georgetown University Medical Center
- 2002-2003
- Postdoctoral Fellow, Department of Radiology, Center for Molecular Imaging Research, Massachusetts General Hospital/ Harvard Medical School

HONORS/ AWARDS
- 2009
- Grant of Japan Orthopaedics and Traumatology Foundation
- 2009
- Asia Traveling fellowship (Japanese Society for Spine Surgery and Related Research) 2009
- 2010
- 1st Cervical Spine Research Society Asia Pacific Section (CSRS-AP) Poster Award 2010
- 2010
- The 25th Annual Research Meeting of the Japanese Orthopaedic Association Poster Award 2010
- 2010
- The 7th Research Meeting of the International Orthopaedic Association NIRA
- 2011
- 1st Keio Intellectual Property Award 2011
- 2012
- The American Academy of Orthopaedic Surgeons (AAOS) Guest Nation Poster Award 2012
- 2012
- The Japanese Orthopaedic Association Encouragement Award 2012
- 2013
- The 59th Annual Research Meeting of Orthopaedic Research Society
- 2015
- Cervical Spine Research Society (CSRS) travelling fellowship 2015
- 2015
- The 30th Annual Research Meeting of the Japanese Orthopaedic Association Poster Award 2015
- 2017
- Scoliosis Research Society Annual Meeting Russell A. Hibbs Basic Research Award
- 2012-present
- Best Doctors in Japan
- 2018-present
- Top Doctors (Sakura no hana) , etc
EDITORIAL BOARD
PLOS ONE: ACADEMIC EDITOR, SIENTIFIC REPORTS: ACADEMIC EDITOR, ASIAN SPINE J: EDITORIAL BOARD, JOURNAL OF ORTHOPAEDIC SCIENCE: EDITORIAL BOARD, CONTEMPORARY SPINE SURGERY: EDITORIAL BOARD, SPINE, SPINE J, SPINE SURGERY AND RELATED RESEARCH (SSRR): EDITORIAL BOARD, ETC
CLINICAL ACHIEVEMENTS
Specialized Fields in Clinical Practice
Dr. Ken Ishii specializes in spinal and spinal cord diseases, orthopedic disorders, and anti-aging treatments for the musculoskeletal system. His expertise in spinal and spinal cord diseases covers a wide range of conditions, including:
- Cervical spine disorders
- Lumbar spine disorders
- Ossification of the posterior longitudinal ligament (OPLL)
- Ossification of the yellow ligament (OYL)
- Degenerative spinal diseases
- Spinal tumors
- Spinal cord and cauda equina tumors
- Spinal arteriovenous fistula (Spinal AVF)
- Spinal deformities such as scoliosis and kyphosis
- Thoracic spinal disorders
- Spinal trauma
- Dropped head syndrome
- Atlantoaxial rotatory fixation (AARF)
- Failed back surgery syndrome (FBSS), etc.
Dr. Ishii’s treatment philosophy is "to prioritize non-surgical methods whenever possible and, when surgery is necessary, to prefer minimally invasive and endoscopic spine surgeries that minimize the burden on the patient."

His team has developed unique conservative therapies that have gained widespread recognition, including:
- SHAiR Program, a specialized rehabilitation program for Dropped Head Syndrome
- Remodeling Therapy for Atlantoaxial Rotatory Fixation (AARF)
- Nerve function improvement blocks
- Nerve function improvement IV therapy
Dr. Ishii has treated over 650 cases of Dropped Head Syndrome, and patients from around the world now seek the SHAiR rehabilitation program he developed. His minimally invasive and endoscopic spine surgeries, as well as other treatments, are performed with exceptional skill, ensuring a low rate of complications, attracting patients globally.
Dropped head syndrome
SHAiR Rehabilitation

SHAiR Rehabilitation
Rehabilitation program for Dropped Head Syndrome “SHAiR ”

Dr. Ishii introduced endoscopic spine surgery to Japan in 1998 and has since mastered various minimally invasive and endoscopic surgical techniques practiced worldwide. He applies these state-of-the-art techniques to the treatment of the conditions listed above.
Key Surgical Expertise
- Minimally Invasive Spine Surgery (MISS/MIS)
- Lateral Interbody Access Surgery
- Endoscopic Spine Surgery (Microendoscopic Surgery (MED), Full-Endoscopic Spine Surgery (FESS))
- Surgery for Ossification of the Posterior Longitudinal Ligament (OPLL) and Yellow Ligament (OYL)
- Total Disc Replacement (TDR)
- Spinal Tumor Resection
- CT-Based Navigation Surgery
As of 2025, Dr. Ishii has performed over 6,500 surgeries, including:
- Approximately 1,650 MIS cervical laminoplasties
- Approximately 2,800 MIS lumbar procedures
- Approximately 500 spinal cord tumor surgeries
- Approximately 650 OPLL and OYL surgeries
With his extensive experience in treating spinal and spinal cord diseases, he has been invited to deliver lectures and conduct surgical training at renowned universities and medical institutions worldwide.
In addition to providing comprehensive treatment for spinal and spinal cord diseases, Dr. Ishii is a pioneer in anti-aging treatments for the musculoskeletal system and actively engages in preventive medicine.
Building on the regenerative medicine techniques he cultivated during his four-year fellowship in the United States, he offers advanced anti-aging and reverse-aging treatments for the musculoskeletal system, including stem cell therapy, backed by extensive research and clinical experience.
Dr. Ishii continues to lead the advancement of minimally invasive spinal treatments and regenerative medicine, contributing to better patient outcomes and innovative approaches to spinal care worldwide.

For more details, click here.
Minimally Invasive Spinal Treatment (MIST)
History and development of Percutaneous PedicleScrew System
SURGICAL COMPLICATION RATES of Dr. Ishii`s PROCEDURES (Past 5 years)
- MIS Cervical Laminoplasties (Minimally Invasive Expansive Laminoplasty (ELAP))
Hematoma: 1.5%
Surgical Site Infection: 0%
C5 Palsy: 2.2%
Reoperation Rate Within One Month Post-Surgery: 1% - Lumbar Endoscopic Surgery (MED, MEL, FESS, DPEL)
Hematoma: 3.3%
Surgical Site Infection: 0%
Dural Tear: 0%
Nerve Injury: 0%
Reoperation Rate Within One Month Post-Surgery: 0% - MIS Lateral Interbody Fusion (LIF) with Percutaneous Pedicle Screw (PPS)
Hematoma: 0%
Surgical Site Infection: 0%
Dural Tear: 0%
Postoperative Iliopsoas Muscle Weakness at Two weeks: 4.5%
Nerve Injury: 0%
Vascular Injury: 0%
Bowel Injury: 0%
Ureteral Injury: 0%
Reoperation Rate Within One Month Post-Surgery: 0%
FACULTY EXPERIENCE at INTERNATINAL MEDICAL INSTITUIONS
- Ishii K. How to MIS-TLIF. Spine Microsurgery Approach Hand-on Cadaveric Workshop(MIS-PLIF), Bangkok, Thailand, 2008.
- Ishii K. World Congress of Minimally Invasive Spine Surgery & Techniques (WCMISST) Industrial Workshop (MIS-TLIF)Faculty, Hawaii, USA, 2008.
- Ishii K. MIS-TLIF: Surgical Procedures and Outcomes. Hands-on Cadaver Lab for Japanese New Spinal Techniques(MIS-TLIF), Memphis, USA, 2009.
- Ishii K. Surgical Procedures of MIS-PLIF. MIS Cadaver Workshop, New York, USA, 2009.
- Ishii K. MIS-TLIF: Surgical Procedures and Outcomes. Worldwide Headquarters Cadaver Workshop, Boston, USA, 2009.
- Ishii K. Trauma in the Occipital Cervical Zone Spine Across the Sea 2009, Hawaii, USA, 2009.
- Ishii K. Spine Cadaver Workshop Program in BKK(MIS-TLIF)Faculty, Bangkok, Thailand, 2010.
- Ishii K. Scoliosis Research Society (SRS) Pre-meeting Course; Management of cervical lesions in pediatric patients: Management of atlantoaxial rotatory fixation, Kyoto, Japan, 2010.
- Ishii K. Spine Cadaver Workshop Program in MIS-TLIF Faculty, Soul, Korea, 2010.
- Ishii K. Spine Cadaver Workshop Program in University of Malaysia (Faculty), Kuala Lumpur, Malaysia, 2011.
- Ishii K. MIS-TLIF Cadaver Workshop Regional Faculty, Singapore, 2011.
- Ishii K. Spine Cadaver Workshop Program in BKK(MIS-TLIF)Faculty, Bangkok, Thailand, 2011.
- Ishii K. Cadaver Workshop Training Faculty, Bangkok, Thailand, 2011
- Ishii K. Advanced Technical Workshop & Hands-on Cadaver Training Faculty, Memphis, USA, 2012.
- Ishii K. Minimally invasive spine surgery (MISS) -past, present & future-. The 13th Annual Meeting of the PASMISS, Miyazaki, Japan, 2013.
- Ishii K. Spine Cadaver Workshop Program in BKK(MIS-TLIF)Faculty, Bangkok, Thailand, 2013.
- Ishii K. Minimally Invasive Cadaver Workshop Program in BKK Faculty, Taipei, Taiwan, 2013.
- Ishii K. Spine Cadaver Workshop Program for Asian surgeons in BKK(MIS-TLIF)Faculty, Bangkok, Thailand, 2013.
- Ishii K. Minimally invasive spine surgery (MISS) -past, present & future-. Asian-pacific Cadabor training, Bangkok, Thailand, 2013.
- Ishii K. Diagnosis and management of chronic atlantoaxial rotary fixation. 2nd International Spine Symposium of 4 Universities/5th JST Orthopedics forum-spine session, April.25-26; Beijing, China, 2014.
- Ishii K. Surgical outcomes of corrective fusion surgeries for dropped head syndrome. 3rd International Spine Symposium of 4 Universities, March.21, Tokyo (Keio Univ Mita Campus), Japan, 2015.
- Ishii K. Surgical outcomes of corrective fusion surgeries for dropped head syndrome. Thomas Jefferson University/Rothman Institute, April.23, Philadelphia, USA, 2015. CSRS traveling fellowship
- Ishii K. Surgical outcomes of corrective fusion surgeries for dropped head syndrome. CMC & OrthoCarolina, April.30, Charlotte, USA, 2015. CSRS traveling fellowship
- Ishii K. Management of Atlantoaxial Rotatory Fixation. CMC & OrthoCarolina, April.30, Charlotte, USA, 2015. CSRS traveling fellowship
- Ishii K. The Incidence of C5 Palsy in Open Door Laminoplasty. Hospital for Special Surgery, May.3, New York, USA, 2015. CSRS traveling fellowship
- Ishii K. Surgical outcomes of corrective fusion surgeries for dropped head syndrome, Toronto Western Hospital, May.12, Toronto, Canada, 2015. CSRS traveling fellowship
- Ishii K. Management of Atlantoaxial Rotatory Fixation –Case Presentation–. Toronto Western Hospital, May.13, Toronto, Canada, 2015. CSRS traveling fellowship
- Ishii K. MIS TLIF vs Open TLIF: Why MIS TLIF matters? Asia Pacific Posterior Spine MIS Instructional Course, Jan.26, Bangkok, Thailand, 2016
- Ishii K. What’s New: Sacral-Alar-Iliac (SAI) technique for sacropelvic fixation Introduction. Asia Pacific Posterior Spine MIS Instructional Course, Jan.27, Bangkok, Thailand, 2016
- Ishii K. MIS-TLIF reduces an incidence of adjacent disc disease in the patients with degenerative spondylolisthesis-comparative study with convention TLIF. 4th International Spine Symposium of 4 Universities, June 4, San Francisco, USA, 2016.
- Ishii K. Overview of MIS Adult Deformity: Challenges vs Solution. 1st ASPAC MIS Expert Panel, Tokyo, 2016.
- Ishii K. Minimally Invasive Spine Surgery: Current and Future Prospects. 7th MIS symposium, Shanghai, China, 2016.
- Ishii K. Avoidance for radiation exposure in MISt. 2nd SOLAS Japan Regional Meeting (Nov. 10, 2018 Nagoya)
- Ishii K. Minimally Invasive Spinal Stabilization (MISt). 2019 China-Japan-ROK Minimal Invasive Spine Surgery Summit, Beijing, China 2019
- Ishii K. Dropped head syndrome-its epidemiology, diagnosis, and treatment. 1st Annual Meeting of Cervical Spine Research Committee affiliated with Korean Society of Spine Surgery (CSRC). Mar 26, WEB, 2021
- Ishii K. Morning Seminar 1 [Minimally invasive spinal treatment: current and future prospects]. 13th Combined Meeting of Asia Pacific Spine Society & Asia Paediatric Prthopaedic Socety (APSS-APPOS) June 11, WEB,2021
- Ishii K. Video on Key Surgical Techniques 1 [Mobi-C total disc replacement -surgical techniques and clinical outcomes-]. 13th Combined Meeting of Asia Pacific Spine Society & Asia Paediatric Prthopaedic Socety (APSS-APPOS) June 11, WEB,2021
- Ishii K. Dropped head syndrome -its epidemiology, diagnosis, and treatment-. Korean Society of Spine Surgeons (KSSS) June 11, WEB,2021
- Ishii K. Faculty Lecture1-3 [Medical reform of navigation technology in minimally invasive spinal treatment (MIST)]. The 21st Annual Meeting of the Pacific and Asian Society of Minimally Invasive Spine Surgery (PASMISS). July 2, WEB, 2021
- Funao H, Yokosuka K, Ukai J, Nakanishi K, Paku M, Tomita T, Hoshino M, Saito T, Ishii K, Sato K.Faculty Lecture. Minimally invasive trans-sacral canal plasty for failed back surgery syndrome.The 21st Annual Meeting of the Pacific and Asian Society of Minimally Invasive Spine Surgery (PASMISS). July 2, WEB, 2021
- Funao H, Yamanouchi K, Fujita N, Kato S, Otomo N, Isogai N, Sasao Y, Ebata S, Ishii K. Antiseptic Meterials. The 1st Annual Meeting of Society for Minimally Invasive Spine Surgery Asia Pacific (SMISS-AP) (Sep. 29-Oct. 1, 2021 Korea) invited speaker
- Ishii K. Advancements in Minimally Invasive Spine Surgery: Efficacy and impact of minimally invasive spine stabilization. ASIA PACIFIC ORTHOPAEDICS, Nov 11, WEB, 2021
- Ishii K. Efficacy and impact of minimally invasive spinal treatment (MIST) in an aged society.7th World Congress of Minimally Invasive Spine Surgery & Techniques (WCMIST), Nov 24th, Tokyo, 2021
- Funao H, Isogai N, Igawa T, Ishii K. Clinical Updates on Dropped Head Syndrome. The 24th Seminar of the Study Group for Nerve and Spine「Spinal Disorders: Updates in Diagnosis and Management」 (Mar. 19-20, 2022 web)
- Ishii K. Dropped head syndrome: Surgical Management for Intractable Cases of Cervical Disorder. 50th Annual Meeting Pre-Conference Sessions (San Diego), Nov. 14, 2022, Web
PUBLICATIONS & PRESENTATIONS
Pathophysiology, Diagnosis, Treatment, and Rehabilitation (SHAiR Program) of Dropped Head Syndrome
1) Introduction
Dropped Head Syndrome (DHS) is a relatively new disease in the field of cervical disorders. It is more common in elderly women over the age of 70, and externally, it manifests as the head drooping forward, making it difficult to look straight ahead. Accurate diagnosis and appropriate conservative treatment, particularly rehabilitation through the SHAiR Program, have been proven effective. Early consultation with an orthopedic specialist is highly recommended before the condition progresses.
2) Cervical Disorders and Symptoms
Long hours of smartphone or computer use, as well as sleeping in an incorrect position, can sometimes cause neck or back pain. In most cases, these symptoms improve within a few days and are considered simple muscle strain or neck stiffness. However, in August 2022, Nobu from the Japanese comedy duo "Chidori" was diagnosed with vertebral artery dissection after experiencing severe neck pain. This condition occurs when the inner lining of the vertebral artery tears, and in severe cases, it can lead to subarachnoid hemorrhage or cerebral infarction, making it a potentially life-threatening disease.
There are various cervical disorders, most commonly cervical disc herniation and cervical spondylosis, which are age-related degenerative diseases. Other conditions include ossification of the posterior longitudinal ligament (OPLL), pyogenic spondylitis, and cervical tumors, among others. Since these diseases involve abnormalities in the cervical bones, muscles, or nerves, they are generally accompanied by neck pain. Additionally, movements such as turning the neck may exacerbate the pain, and in some cases, symptoms like radiating pain or numbness in the arms, shoulders, or legs may develop. If the spinal cord is significantly compressed within the cervical spine, nerve dysfunction can occur, leading to muscle weakness, impaired balance and walking difficulties, and, in severe cases, bladder and bowel dysfunction.
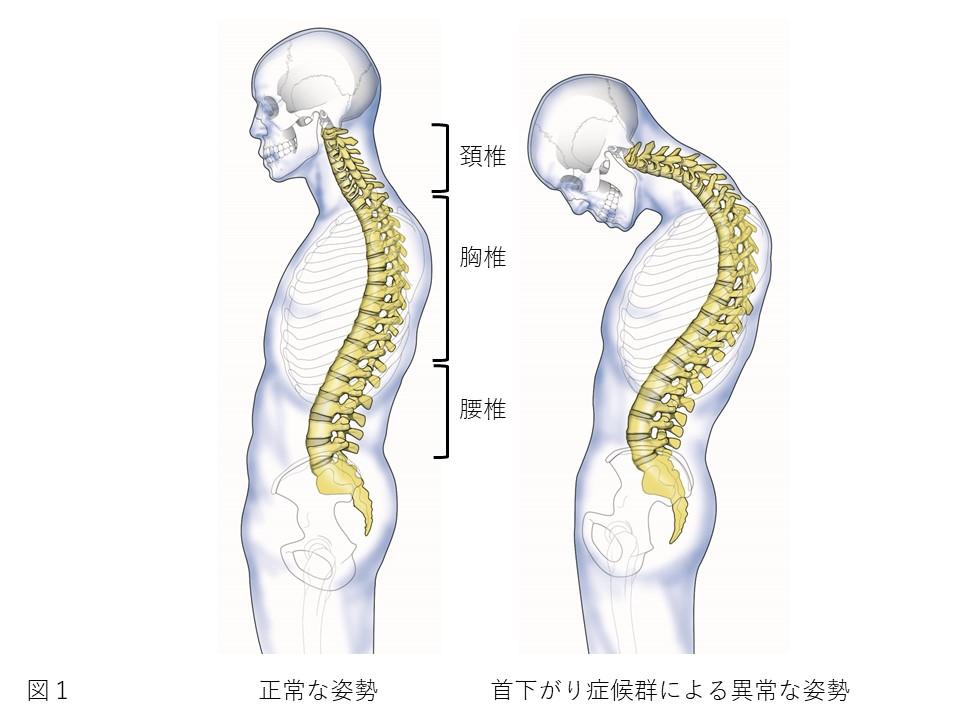
3) What is Dropped Head Syndrome (DHS)?
In 1887, a Japanese researcher was the first in the world to report a condition called "Kubisagari" (literally translated as "drooping neck"). More than 100 years later, in 1992, a set of symptoms characterized by severe dysfunction of the cervical extensor muscles (muscles that extend the neck backward) was named Dropped Head Syndrome (DHS). This means that DHS is a relatively new disease concept.
DHS is most commonly seen in elderly women over the age of 70. Visually, the neck or upper back bends forward, causing the head to droop, which leads to difficulty looking straight ahead, a symptom known as "horizontal gaze impairment."
In actual clinical practice, around 2005, Dr. Ken Ishii at Keio University Hospital saw only a few cases per year of DHS. Until recently, the condition was considered relatively rare. However, with the advancement of Japan’s super-aging society and increasing awareness among doctors, many previously undiagnosed patients are now visiting hospitals for consultation.
Currently, Dr. Ishii treats approximately 650 patients with DHS, with 4 to 5 new patients referred to his clinic from across the country at every outpatient session. Interestingly, Dr. Ishii has noted that Japan has a significantly higher number of DHS patients compared to other Asian countries, the United States, and Europe. This may be due to cultural, lifestyle, or genetic factors, which require further investigation.
4) Causes and Symptoms
The causes of Dropped Head Syndrome vary and can be classified into several categories:
- Idiopathic (Unknown cause)
- Post-traumatic (After injury)
- Post-surgical (After cervical spine surgery)
- Neurological diseases (e.g., Parkinson’s disease, Amyotrophic Lateral Sclerosis (ALS), Stroke)
- Endocrine disorders (e.g., Hypothyroidism)
- Psychiatric conditions (e.g., Depression)
- Autoimmune diseases (e.g., Rheumatoid arthritis)
According to Dr. Ishii’s clinical research team, approximately 70% of cases are idiopathic, meaning the cause is unknown. However, it is presumed that age-related postural changes and muscle weakness in the neck may contribute to its development.
The primary symptom of DHS is horizontal gaze impairment, making it difficult for patients to look straight ahead. However, continuous drooping of the head throughout the entire day is rare. Many patients report that:
- The condition worsens in the afternoon but is normal in the morning
- Head drooping occurs only while walking, but improves when sitting down
Other associated symptoms include:
- Neck pain (stiff neck) and shoulder pain
- Gait disturbances due to neck posture
- Swallowing difficulties (dysphagia)
- Jaw opening difficulties (trismus), leading to eating difficulties
In severe cases, the spinal cord or nerve roots may be compressed, causing:
- Paralysis in the limbs
- Severe weakness in the arms or legs
- Loss of bladder and bowel control
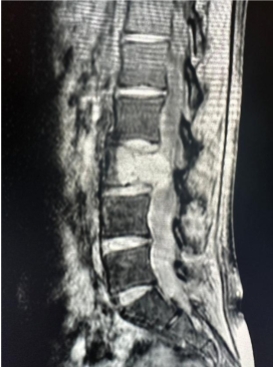
5) Diagnosis
Diagnosing DHS is relatively straightforward. The hallmark feature is a forward-drooping head posture during sitting, standing, or walking. However, identifying the underlying cause requires detailed examination and extensive clinical experience, making definitive diagnosis challenging.
To differentiate DHS from other conditions, doctors must rule out:
- Fractures and spinal cord injuries (trauma-related conditions)
- Ankylosing spondylitis
- Diffuse idiopathic skeletal hyperostosis (DISH)
- Ossification of the posterior longitudinal ligament (OPLL)
- Spinal tumors
- Congenital cervical spine abnormalities
Common diagnostic tests include:
- X-rays (to assess spinal alignment and bending points)
- CT scans (for bony structures and abnormalities)
- MRI scans (to examine nerve and soft tissue damage)
- Blood tests (to check for neurological or autoimmune disorders such as Parkinson’s disease)
Because DHS can mimic other diseases, an experienced specialist is necessary for an accurate diagnosis.
6) Treatment Strategy
The treatment approach depends on the underlying cause. However, identifying the exact cause at the onset of DHS is often difficult. In rare cases, DHS improves spontaneously within a few weeks, but for most patients, the condition remains unchanged for months or years.
Unfortunately, many patients do not receive proper treatment. They are often misdiagnosed with age-related posture changes and prescribed painkillers or general rehabilitation as a temporary measure. Due to the rarity of the disease, very few physicians in Japan have extensive experience treating DHS.
In confirmed cases of DHS, conservative treatments such as bracing, medication, and rehabilitation are the primary options. A minimum of three months of conservative therapy is typically recommended. However, dramatic improvements are rare, which is a globally recognized issue in DHS treatment.
In some cases, DHS can be progressive, leading to:
- Difficulty opening the mouth and swallowing
- Nutritional deficiencies
- Increased risk of becoming bedridden
In such cases, surgical treatment may be necessary, depending on the patient’s condition and quality of life.
7) Effectiveness of Conservative Treatment
For DHS patients without nerve paralysis or life-threatening conditions, conservative treatments such as bracing and rehabilitation are preferred.
-
Bracing therapy:
- Helps maintain a forward-facing posture
- Improves daily activities (ADL)
-
Rehabilitation therapy:
- Strengthens paraspinal and cervical extensor muscles
- Improves spinal mobility and posture control
However, traditional rehabilitation programs have shown limited success. Only about 5-20% of patients show improvement, and symptoms often return once therapy stops.
Recognizing this limitation, Dr. Ishii’s clinical team developed a novel rehabilitation method: the Short and Intensive Rehabilitation (SHAiR) Program. This program includes:
- Targeted muscle strengthening for neck and trunk muscles
- Postural adjustment and flexibility training
- Pelvic tilt exercises
- Gait training
Unlike conventional programs, SHAiR has demonstrated a success rate of approximately 90%, making it a breakthrough in DHS rehabilitation. However, continued therapy at home is crucial for long-term benefits.
8) Surgical Treatment for Dropped Head Syndrome
Indications for surgery
Surgical treatment for DHS is considered when:
- Nerve paralysis is present
- Horizontal gaze impairment significantly reduces the patient’s quality of life (QOL)
- Severe jaw opening restriction or swallowing difficulties (dysphagia) lead to eating problems
If conservative treatments (such as bracing and rehabilitation) fail to improve symptoms, surgery may be necessary to restore functional posture and prevent further complications.
Surgical procedure
The standard surgical approach for DHS is posterior cervical fixation, which involves:
- Making an incision in the back of the neck
- Placing implants on the cervical vertebrae to realign and stabilize the neck
- Correcting spinal alignment for optimal head positioning
In cases where severe spinal deformity is present, an anterior approach (incision in the front of the neck) may be required to realign the cervical spine before performing posterior fixation.
Dr. Ishii has performed over 85 surgical cases of DHS with generally favorable outcomes. However, like any surgery, risks and complications exist, and patients should discuss the procedure thoroughly with their physician beforehand.
9) Summary
This document has provided an overview of:
- The structure of the cervical spine
- Common cervical disorders and symptoms
- Pathophysiology, diagnosis, and treatment of Dropped Head Syndrome (DHS)
- The importance of early diagnosis and appropriate conservative treatment
Particularly, the SHAiR Program, developed by Dr. Ishii’s clinical team, has demonstrated exceptional effectiveness, making it a strongly recommended treatment option for DHS patients. The SHAiR Program has achieved a 90% success rate, making it one of the most effective rehabilitation methods available worldwide. Future research will continue to focus on raising awareness, refining treatment strategies, and improving patient outcomes for DHS.
However, if conservative therapy fails, patients with severe disability, eating disorders, or life-threatening conditions may require surgical intervention to improve their daily functioning and overall prognosis.
Moving forward, continued research, awareness, and treatment optimization for DHS remain crucial in advancing patient care and improving clinical outcomes.
10) SHAiR Program: Before & After Comparison
Before the SHAiR Program
After the SHAiR Program
Publications by Dr. Ishii’s clinical team
1. Development of a Novel Rehabilitation Program for Dropped Head Syndrome
📄Igawa T, Isogai N, Suzuki A, Kusano S, Sasao Y, Nishiyama M, Funao H, Ishii K.
Establishment of a novel rehabilitation program for patients with dropped head syndrome: Short and intensive rehabilitation (SHAiR) program.
J Clin Neurosci. 2020
- Corresponding Author: Dr. Ken Ishii
Surgical treatment was previously considered the only viable option for DHS, as conservative methods showed limited effectiveness. Dr. Ishii’s team developed a new rehabilitation program, SHAiR, which includes:
- Neck strengthening exercises
- Postural and flexibility training
- Pelvic tilt and gait exercises
This study found that SHAiR significantly outperformed traditional rehabilitation methods in reducing neck drooping and pain. It was the first study in the world to provide scientific evidence supporting the effectiveness of rehabilitation for DHS patients.
2. Effects of SHAiR on Walking Posture in DHS Patients
📄Suzuki A, Ishii K, Igawa T, Isogai N, Ui H, Urata R, Ideura K, Sasao Y, Funao H.
Effect of the short and intensive rehabilitation (SHAiR) program on dynamic alignment in patients with dropped head syndrome during level walking.
J Clin Neurosci. 2021
- Corresponding Author: Dr. Ken Ishii
Although SHAiR was proven effective in improving static posture, its effects during walking movement had not been studied. Using a 3D motion capture system, the research team analyzed gait changes before and after SHAiR treatment.
- Patients who completed SHAiR showed significant improvement in head posture and walking efficiency
- They were able to take longer steps and maintain a more upright posture while walking
This study demonstrated that SHAiR is not only effective in standing posture but also improves dynamic movement and walking mechanics.
3. Relationship Between Sarcopenia and DHS
📄Igawa T, Ishii K, Suzuki A, Ui H, Urata R, Isogai N, Sasao Y, Nishiyama M, Funao H.
Prevalence of sarcopenia in idiopathic patients is similar to healthy volunteers.
Sci Rep. 2021
- Corresponding Author: Dr. Ken Ishii
Sarcopenia (muscle loss) has been linked to DHS, but previous studies suggested that DHS patients had higher rates of sarcopenia than healthy individuals.
Using new diagnostic criteria, this study found that:
- DHS patients had similar sarcopenia rates as healthy individuals
- DHS patients had normal limb muscle mass but showed reduced core muscle mass
These findings challenge previous assumptions and highlight that DHS is not solely caused by general muscle loss but may involve specific muscle imbalances.
4. The Impact of SHAiR on Dynamic Walking Mechanics in DHS Patients
📄Igawa T, Ishii K, Urata R, Suzuki A, Ui H, Ideura K, Isogai N, Sasao Y, Funao H.
Dynamic alignment changes during level walking in patients with dropped head syndrome: analysis using a three-dimensional motion analysis system.
Sci Rep. 2021
- Corresponding Author: Dr. Ken Ishii
Using 3D motion capture, researchers found that:
- DHS patients had shorter strides and an increased backward tilt of the body while walking
- DHS patients showed weak propulsion from the ground, leading to inefficient gait mechanics
This study provided critical insights into walking impairments in DHS patients and supported the role of SHAiR in improving walking mechanics.
5. The Relationship Between Horizontal Gaze Ability and Physical Function in DHS Patients
📄Igawa T, Ishii K, Urata R, Suzuki A, Ui H, Ideura K, Isogai N, Sasao Y, Funao H.
Association between the Horizontal Gaze Ability and Physical Characteristics of Patients with Dropped Head Syndrome.
Medicina. 2022
- Corresponding Author: Dr. Ken Ishii
- Horizontal gaze impairment was strongly correlated with gait speed and spinal posture
- Interestingly, neck muscle strength was not a major factor in gaze impairment
This study challenged previous beliefs about the role of neck muscle strength in DHS and suggested that gait ability and posture were more critical factors in maintaining normal head position.
6. The Potential Efficacy of Serotonin-Noradrenaline Reuptake Inhibitor Duloxetine in Dropped Head Syndrome: A Case Report and Review of the Literature
📄Funao H, Isogai N, Ishii K.
The potential efficacy of serotonin noradrenaline reuptake inhibitor duloxetine in dropped head syndrome: A case report and review of the literature.
Heliyon. 2020 Aug 22;6(8):e04774. doi:10.1016/j.heliyon.2020.e04774.
- Corresponding Author: Dr. Ken Ishii
Title: The Potential Efficacy of Duloxetine (Serotonin-Noradrenaline Reuptake Inhibitor) in Dropped Head Syndrome: A Case Report and Literature Review
When Dropped Head Syndrome (DHS) is caused by neurological disorders such as Parkinson’s disease or amyotrophic lateral sclerosis (ALS), pharmacological treatment is the first-line approach. However, when the cause remains unknown, there is currently no established medication for DHS.
Duloxetine, a serotonin-noradrenaline reuptake inhibitor (SNRI), is commonly prescribed for chronic musculoskeletal pain, neuropathic pain, and depression. In this study, a 70-year-old female DHS patient with severe neck pain was treated with duloxetine, which resulted in:
- Reduction of neck pain
- Improvement in horizontal gaze impairment
- Resolution of gait disturbances
The potential mechanisms behind these improvements include:
- Pain relief, allowing the patient to move her neck more freely.
- Modulation of serotonin and noradrenaline, which may have positively influenced DHS symptoms, improving muscle control and postural stability.
This case report suggests that duloxetine may be a viable pharmacological treatment for DHS patients with an unknown etiology.
7. The Short and Intensive Rehabilitation (SHAiR) Program Improves Dropped Head Syndrome Caused by Amyotrophic Lateral Sclerosis: A Case Report
📄Urata R, Igawa T, Suzuki A, Sasao Y, Isogai N, Funao H, Ishii K.
The Short and Intensive Rehabilitation (SHAiR) Program Improves Dropped Head Syndrome Caused by Amyotrophic Lateral Sclerosis: A Case Report.
Medicina (Kaunas). 2022 Mar 21;58(3):452. doi: 10.3390/medicina58030452.
- Corresponding Author: Dr. Ken Ishii
Title: Short and Intensive Rehabilitation (SHAiR) Program Improves Dropped Head Syndrome (DHS) Caused by Amyotrophic Lateral Sclerosis: A Case Report
Amyotrophic lateral sclerosis (ALS) is one of the known causes of Dropped Head Syndrome (DHS). While the SHAiR rehabilitation program has been shown to be effective in idiopathic DHS, its impact on ALS-related DHS has not been well documented.
In this study, a 70-year-old male ALS patient underwent SHAiR rehabilitation for two weeks, with the following results:
- Progressive improvement in forward gaze impairment within the first week
- Near-complete resolution of DHS symptoms after two weeks
- Significant reduction in neck pain and improvement in quality of life (QOL)
Traditionally, patients with ALS-related DHS have been limited to brace therapy. However, this case report suggests that SHAiR may be a promising non-surgical treatment option even for ALS-related DHS cases.
8. Association Between the Phase Angle and the Severity of Horizontal Gaze Disorder in Patients with Idiopathic Dropped Head Syndrome: A Cross-Sectional Study
📄Urata R, Igawa T, Ito S, Suzuki A, Isogai N, Sasao Y, Funao H, Ishii K.
Association between the Phase Angle and the Severity of Horizontal Gaze Disorder in Patients with Idiopathic Dropped Head Syndrome: A Cross-Sectional Study.
Medicina (Kaunas). 2023 Mar 8;59(3):526. doi: 10.3390/medicina59030526.
- Corresponding Author: Dr. Ken Ishii
Title: Association Between the Phase Angle and Horizontal Gaze Disorder in Patients with Idiopathic Dropped Head Syndrome: A Cross-Sectional Study
The phase angle is a biomarker of cellular health, recently gaining attention in the medical field. It has been associated with physical functions in older adults, including standing ability, leg strength, and walking speed. However, its relationship with horizontal gaze impairment in DHS has not been studied before.
This study compared the phase angle between DHS patients and healthy controls, matched for age, height, and lean body mass. The findings revealed:
- DHS patients had a significantly lower phase angle compared to healthy individuals
- Phase angle was strongly associated with the severity of horizontal gaze impairment
Interestingly, neck muscle strength, previously believed to be a key factor in DHS, was not significantly related to gaze impairment.
This study was the first in the world to demonstrate a relationship between phase angle and DHS severity, suggesting that cellular health and systemic muscle function play a crucial role in DHS pathology.
9. Effect of individual spinal muscle activities on upright posture using a human body finite element model
📄Nakahira Y, Iwamoto M, Igawa T, Ishii K
Effect of individual spinal muscle activities on upright posture using a human body finite element model
Sci Rep 2025 doi.org/10.1038/s41598-025-86788-0
- Corresponding Author: Dr. Ken Ishii
Diseases with abnormal spinal alignment, such as kyphosis, lordosis, scoliosis, and dropped head syndrome (DHS), are increasingly common, especially in older adults. DHS is characterized by excessive forward tilt of the head and neck, leading to difficulty in lifting the head and symptoms like neck pain, impaired flexion, difficulty walking, eating, dysphagia, and skin ulcerations. Causes include neurological disorders, muscle diseases, and cervical spondylosis, but the exact mechanism remains unclear.
Treatment options include surgery, orthotic devices, pharmacotherapy, and physical therapy, with cervical extension exercises showing effectiveness. However, the mechanisms remain poorly understood. To investigate this, a finite element human body model was used, simulating muscle activation in posture maintenance. The study found that trunk extensors (multifidus L1-S, longissimus thoracis) and hip flexors (psoas major, iliacus) are crucial for posture stability, supporting previous rehabilitation findings. Further research on muscle activity and treatment mechanisms could improve DHS management.